How a Dental Office Controls Infections
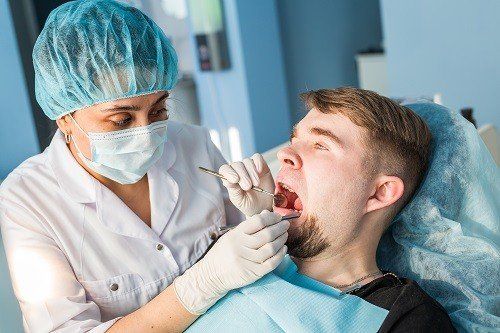
Whether they’re filling cavities, performing root canals, or just cleaning patients’ teeth, dental professionals are trusted with the health and care of their patients’ mouths and providing essential services we cannot perform ourselves. However, how often do we think about the circumstances in which dental professionals work and what it takes to keep that environment clean and infection-free? For your knowledge, here is what you should know about infection control in a dental office.
Equipment and Instrument Cleaning
The CDC makes it clear how dental equipment and instruments should be disinfected and cleaned. Equipment and instruments are classified using one to three groups based on the risk of transmitting infections:
1. Critical : This category designates instruments that are used for penetrating bone or soft tissue and that encounter blood as well. Instruments with this designation include scalpels, scalers, bone chisels, and forceps. Critical instruments must be sterilized following every use via autoclaving, chemical/heat vapor, or dry heat.
2. Semi-critical : These instruments encounter non-dry skin or mucous membranes, including the inside of cheeks. Such instruments include amalgam condensers, mirrors, and reusable impression trays, and they should be sterilized after every use via dry heat.
3. Non-critical : These types of instruments only touch intact skin, including X-ray heads, pulse oximeters, and blood pressure cuffs. These instruments may be reused in between patients once they’ve received a low-level or intermediate-level disinfection.
Hand Washing
The act of hand washing is crucial for the prevention of diseases spreading. Alcohol-based hand-sanitizing solutions, per the CDC, can be utilized most of the time except whenever hands are visibly covered in debris or dirt. Dental professionals with visibly dirtied hands need to wash with water and soap, with the CDC recommending hand washing in one of four scenarios:
- The dental professional’s hands are clearly and visibly dirtied.
- The dentist has touched equipment with bare hands that could be contaminated by saliva, blood, and similar secretions.
- After and before the dentist has treated a patient.
- Before the dentist has put gloves on and immediately after their removal.
Office Cleanliness and Surface Contamination
Infection prevention and surface contamination applies to much more than dental instruments. Dental offices, per the CDC, contain two kinds of surfaces—housekeeping surfaces and clinical contact surfaces. Regarding housekeeping surfaces, this includes walls, sinks, and floors, and research suggests they offer little to no risk of contamination as long as they are regularly cleaned with water and detergent. Floors, however, must be cleaned more regularly than other housekeeping surfaces, per the CDC.
For clinical contact surfaces, these include items like drawer handles, light handles, countertops, chairs, faucet handles, and other objects patients or dentists might touch during procedures. If they’re not protected via barriers like sheets, bags, or plastic wrap, clinical contact surfaces must be cleaned in between patients using EPA-registered hospital disinfectants. These surfaces should be cleaned when workdays have ended.
Training and Education
Dental offices offer ongoing training and education to employees in order to ensure procedures and policies are correctly practiced. The CDC also recommends that training cover safety rules for both patients and employees. As with any business, dental offices need to maintain records of cleanliness and safety training, as is required by state and federal governments.
If you are avoiding the dentist due to the high costs of dental care, our NH supplemental dental insurance can help. To learn more about our plans or to sign up for coverage, click here.